Posted by Gibbeum Hospital
Kang Repair
Non-Mesh Tissue Repair
Kang repair is a new inguinal hernia repair method that does not use mesh at all. The skin incision is made about 3~3.5cm in size transversely at the inguinal area. In some hospitals that do tissue repairs, oblique skin incisions are made but with poor results cosmetically.
Tailored repair
One of the big differences between older tissue repairs and the new Kang repair is this; in older tissue repairs, they perform the same repair method for both indirect and direct inguinal hernias, while Kang repair has two distinct procedures for indirect and direct inguinal hernias, respectively.
There are two types of inguinal hernia – indirect and direct type. The distinction between indirect inguinal hernias and direct inguinal hernias is based on where they occur in relation to inferior epigastric vessels which run along the middle of the inguinal canal obliquely. The inferior epigastric vessels which run along the inguinal canal act as a border between two parts, the superolateral and inferomedial zones. The indirect inguinal hernia occurs through the internal inguinal ring which is located at the superolateral zone, while the direct inguinal hernia occurs through the torn floor muscle of the Hesselbach triangle of the inferomedial zone which is called the posterior wall.
Although the indirect and direct types occur in very different areas, the older tissue repairs adopt the same procedure which reinforces the posterior wall for both types of hernias. So, the older tissue repairs are called posterior wall repairs. Although they try to fix the superolateral zone by extending the posterior wall repair upwardly, it is not sufficient for the indirect inguinal hernia which occurs at the superolateral zone of the inguinal canal. However, Kang repair has two distinctively tailored repair methods, Kang repair for indirect inguinal hernias and Kang repair for direct inguinal hernias respectively. For direct inguinal hernias, we perform a similar procedure to the posterior wall repair. But it is much simpler because the fixing procedure is limited to the Hesselbach triangle without extending upwardly. For indirect inguinal hernias, we just close the internal inguinal ring, the hernia ring directly by the stitching. We don’t fix the Hesselbach triangle for indirect inguinal hernias at all.
The older tissue repairs, so-called posterior wall repairs, showed very high recurrence rates of between 10-30%. Doctors believed that the high recurrence in the posterior wall repair was due to the tension produced by stitching the muscles together to conceal the hernia hole. So they started to insert mesh cloth to conceal the hernia hole instead of pulling and stitching separate muscles together. But we don’t agree with that idea. We believe the main cause of the high recurrence from posterior wall repair surgery is the lack of tailored methods for the different types of inguinal hernias. As a result, the indirect hernia was repaired incorrectly during old posterior wall repairs. So, we believe that not mesh but a tailored repair method is the solution to lowering the high recurrence rate of the posterior wall repairs without occasional debilitating complications.
Reliable Treatment of the Hernia Sac
A hernia sac is formed due to the exit of peritoneum through a gap in the abdominal wall muscle. After exiting through the gap, the peritoneum inflates like a balloon; thus explaining the name, hernia sac. Generally, during indirect inguinal hernia surgery, the hernia sac is separated from the surrounding tissue then tied up where it connects to the peritoneum and then the “sac” is trimmed off. After all that, the tied up, trimmed off part is pushed back in through the muscle gap.
Through extensive surgical experience, we have found that in order to prevent hernia recurrence, it is crucial to push it deep back inside. But unfortunately, previous retroperitoneal repairs did not pay close attention to this step. Properly dealing with the hernia sac is very much important in direct inguinal hernia surgery as well. So, during my Kang Repair, this process is thoroughly carried out. However, regardless of incision or laparoscopic surgery, existing direct inguinal hernia surgeries have overlooked this crucial step and many omit the whole process of dealing with the hernia sac. I believe that it is a factor that drastically increases the risk of recurrence. Properly dealing with the hernia sac by pushing it back deep inside through the gap in the muscle is one of several important aspects of Kang Repair.
Direct Closure
In regards to Kang repair for indirect hernia, we just identify the internal inguinal ring, which is a hernia hole, and close it directly by stitching. We don’t fix the Hesselbach triangle at all. But the posterior wall repair method reinforced mainly the Hesselbach triangle area, with some upward extension around the internal inguinal ring even for indirect inguinal hernias.
Kang repair for indirect hernia is similar to the one described by Dr. Marcy in the past, but modified to avoid the high recurrences. In fact, most of the internal inguinal ring is occupied by the spermatic cord which contains the testicular vessels, lymphatics and sensitive nerves. So it is very difficult to close the internal inguinal ring securely without damaging the aforementioned sensitive structures. That is why this new sort of procedure has not been developed until now. Kang repair for direct hernia also modified the older posterior wall repair methods to minimize damage to surrounding structures and to make the repair stronger. In Kang repair for direct hernia, the scope of surgery has been much smaller than in the older posterior wall repairs including Shouldice or Desarda. In conclusion, another characteristic of Kang repair is that it minimizes the scope of surgery and closes the hernia hole directly.
The Least Invasive repair
Kang repair is the least-invasive inguinal hernia repair procedure that has so far been introduced.
Skin wound

First of all, the size of the skin wound is only about 3.5cm(less than 1.5 inches), which is smaller than that of the traditional tissue repairs. Such small wounds are possible because of the tailored repair methods, each modified to the specific types of inguinal hernia. It is larger than the laparoscopic skin wound but the whole abdominal wall layer has to be penetrated in the laparoscopic repairs. So Kang repair is the least invasive because it damages superficial abdominal wall layers only.
Extent of operation
The factor which most influences the degree of invasiveness is the extent of surgery. This is because the larger the scope of surgery, the greater the extent of tissue damage. Kang repair is performed within only a 4x4cm sized wound. Old posterior wall repair is not tailored for each type of inguinal hernia nor covers both zones, and the extent of surgery is much larger than that of the tailored Kang repair. Open mesh repair usually uses a mesh of 5x10cm whilst laparoscopic inguinal hernia repair uses a mesh of 14x10cm in size. The scope of the mesh repair is bound to be larger than the individual mesh size because the mesh should be adjusted and fixed to underlying structures which need extra space to allow the necessary fixing procedure Looking at the above, Kang repair clearly has the smallest operating range and is the least invasive from a surgical point of view.
Operating time
The longer the operating hour is, the more complex the surgical procedure is. Tissue damage continues to occur during the whole surgical operation process. Thus, the length of the operating time and degree of tissue damage are proportional. The laparoscopic hernioplasty takes at least one hour. Open mesh hernia repair or traditional posterior wall repair requires at least 40 minutes. Kang repair, on the other hand, needs no more than 20 to 30 minutes. Kang repair does not require a mesh insertion and fixation during the operation. Thus, compared to any other hernia repair, our operating time is the shortest. In conclusion, Kang repair is the least invasive from the point of view of operating times.
As shown above, when assessing some elements such as the extent of surgery or the operating time, Kang repair is undoubtedly the least invasive inguinal hernia repair ever. The least invasive means there is least likely to be a complication and it means the quickest to achieve recovery.
Under Local Anesthesia
Kang repair is performed without exception under local anesthesia. This is possible because of the small surgery field and the short surgery time. Laparoscopic mesh repair is always performed with general anesthesia. Local anesthesia is generally a very safe method of anesthesia. However, local anesthetics also have a safe range of dosage. If large quantities of local anesthetic are used, the absorbed anesthetic, if over the safe range, can cause various side effects such as cardiac arrhythmia or suppression. The open mesh repairs or traditional posterior wall repairs can also be performed with local anesthesia, but it is difficult to infiltrate enough local anesthetics into the larger operative area for the repairs because of the dosage limitation. For these reasons, open mesh repair or past posterior wall repair is usually performed with spinal or general anesthesia.
For lidocaine, which is widely used as a local anesthesia, the maximum adult dosage is 4.5 mg/kg or 300 mg in total. This is 22.5cc of 1% lidocaine for a 50kg adult and 27cc of 1% lidocaine for a 60kg adult. Even if one’s weight is higher than 67kg, 30cc of 1% lidocaine is the maximum dose allowed. In reality, lidocaine, which is less than 1%, has a less analgesic effect because of its weak potency. It is not easy to infiltrate an area larger than 5x5cm with a 22.5 to 30cc solution. However, the local anesthesia can be used safely only for Kang repair, which has an operating field of just 4x4cm.
It is safe and simple, but some people are a little scared of the pain during the injection. So, we using intravenous sedatives infiltrate local anesthetics into the operative field while the patients are asleep. It allows them to undergo surgery without feeling any pain at all.
Comparison table
| Indirect inguinal hernia | |||||
|---|---|---|---|---|---|
| Mesh repair | Desarda | Most Post wall (corrupt Bassini repair etc) | Bassini repair/ Shouldice reapir | Kang repair | |
| Mesh | Yes | No | No | No | No |
| Hernia hole | Left open | Left open | Left open | Directly closed | Directly closed |
| Main barrier after repair | mesh | New tissue barrier | New tissue barrier | Repaired anstomical barrier | Repaired anatomical barrier |
| Material of main barrier | Sheet of mesh/ 3D mesh | External oblique aponeurosis | Mostly, conjoint muscle and inguinal ligament | Transversalis fascia (whole length from deep inguinal ring to Hesselbach triangle) | Transversalis fascia (stretched deep inguinal ring only) |
| Auxiliary barrier | No | No | No | Conjoint muscle and inguinal ligament (whole inguinal canal) | No |
| Extent of repair | Both | Both | Both | Both | Superolateral zone only |
| Tailored repair | No | No | No | No | Yes |
| Tension | none | less | much | much | less |
| Operating time | >40-60 mins | 40 mins | >40 mins | >40 mins | 20 mins |
| Anesthesia | General | Spinal or local | General or spinal | General or spinal | Local |
| Recurrence rate | 2-3% | ? | 10-30% | 1-2% | <0.5% |
| Complication rate | High | Low | Variable | Variable | Very low |
| Direct inguinal hernia | |||||
|---|---|---|---|---|---|
| Mesh repair | Desarda | Most Post wall (corrupt Bassini repair etc) | Bassini repair/ Shouldice reapir | Kang repair | |
| Mesh | Yes | No | No | No | No |
| Hernia hole | Left open | Partially local | Variable | Directly closed | Directly closed |
| Main barrier after repair | mesh | New tissue barrier | New tissue barrier | Repaired anstomical barrier | Repaired anatomical barrier |
| Material of main barrier | Sheet of mesh/ 3D mesh | External oblique aponeurosis | Mostly, conjoint muscle and inguinal ligament | Transversalis fascia (whole length from deep inguinal ring to Hesselbach triangle) | Transversalis fascia of Hesselbach triangle only |
| Auxiliary barrier | No | Sutured transversalis fascia (purse string suture) | No | Conjoint muscle and inguinal ligament (whole inguinal canal) | Conjoint muscle and inguinal ligament (over Hesselbach triangle only) |
| Extent of repair | Both | Both | Both | Both | Inferomedial zone (Hesselbach triangle) only |
| Tailored repair | No | No | No | No | Yes |
| Tension | none | less | much | much | some |
| Operating time | >40-60 mins | 40 mins | >40 mins | >40 mins | 20 mins |
| Anesthesia | General | Spinal or local | General or spinal | General or spinal | Local |
| Recurrence rate | 2-3% | ? | 10-30% | 1-2% | <0.5% |
| Complication rate | High | Low | Variable | Variable | Very low |
- ― Posterior wall repair: the same procedure for indirect or direct type hernias
- ― Mesh repair: the same or similar procedure for indirect or direct type hernias
Postop course
- Hospitalization : day clinic or overnight admission
- Walking : soon after operation
- Meal : normal meals soon after operation
- Pain killer : 3-4 days
- Taking shower : from the very next day
- Wound care : just changing preformed dressing gauze, no need to remove stitches
- Flight : even the next day is possible
- Back to work : any time, even the next day
- Jogging and swimming : after a week
- 2 weeks later : No need to limit any physical activity, but listen to what your body tells you
Special adhesive for surgery is used on the surgical region and patients do not have to visit the hospital to get treatment on the surgical part or to get stitches removed.
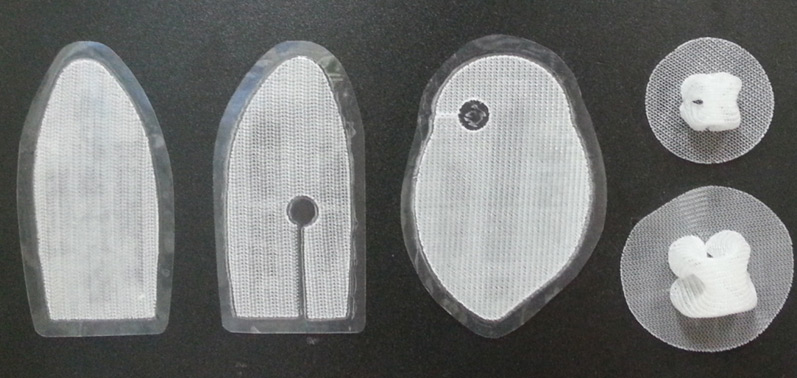
Mesh hernia repair
Mesh is made of chemical fiber woven into various shapes. From the late 1980s, it was first used for inguinal hernia surgery. And today it is the most widely performed inguinal hernia repair worldwide. It is used to cover the inside or outside of a weak area of the inguinal region either through open surgery or by laparoscopic surgery.
Why mesh?
Before mesh operations, a tissue repair method called posterior wall repair was widely performed for inguinal hernia surgery. Surgery is undertaken to reinforce the inguinal canal by pulling and sewing the muscles and ligaments, which are found at the outer layer of the hernia hole, together. This is the barrier which acts to block herniation. But the recurrence rate was very high: 10 to 30%.
Doctors postulated that the high recurrence rate was due to tension at the newly formed barrier. Pulling muscles together to sew creates a repellent force in the direction of the muscles original position. This force is called tension. Eventually, when the force exceeds the limit, the muscle is ripped apart and released. Then, the hernia recurs. In order to avoid tension, they covered it with a tough mesh cloth instead of pulling and stitching, And they thought that by doing this, recurrences could be prevented.
Recurrence rate of mesh repair
Recurrence rates of tissue repair, which were 10-30%, were reduced to as low as 2-5% after the use of mesh. Some of the expected objectives were achieved. But it’s a bit disappointing that there wasn’t a perfect result. As the recurrence rate of 2-5% is still not small. In addition, some studies have suggested that the recurrence rate for mesh hernia repairs is still higher than 10%.
(Niebuhr H and Köckerling F. Surgical risk factors for recurrence in inguinal hernia repair – a review of the literature. Innov Surg Scl 2017;2(2):53-59.)
However, we don’t agree that high recurrence rates are significantly related to tension.
The real problem with mesh
The real problems with mesh hernia repair are not as conspicuous. Although it reduced the recurrence rate, new complications arised by using mesh for inguinal hernia repair.
The most common type of mesh complication is severe chronic pain. At least 10% of patients experience chronic pain after receiving mesh inguinal hernia repair. And many of them are in so much pain that their daily lives are very difficult. In addition, mesh, which is a foreign material, is very vulnerable to bacterial infections. So, there is a chance that pus could later accumulate around the surgical area. Though rare, mesh could migrate and make a hole in the bowel or bladder. In addition, various complications such as nerve damage, foreign body sensations, allergies and pressure have been reported. As a result, a series of lawsuits by patients affected by complications due to hernia mesh continue in many countries. http://www.drugwatch.com/hernia-mesh/
Treatment of mesh sequela
If the sequela is severe, you should undergo surgery to remove the mesh. This operation is very difficult and can damage nearby nerves, blood vessels, and muscles. But it’s a bit disappointing that there wasn’t a perfect result. Moreover, if the mesh was inserted laparoscopically, it is much more difficult to remove it. Therefore, mesh repair gives some reduction in recurrence at the cost of increased complications. If you have a recurrence, you need to get another operation. But when mesh complications occur, you will go through a much more painful situation. In conclusion, mesh hernia repair delivers more setbacks than solutions.

Someone asking for advice with regards to mesh pain
Prevention of mesh complications
What is the best way to prevent mesh complications? It is obviously to stop using mesh. Then, should we go back to the old tissue repair method? The high rate of recurrences effectively rules out going back to that method. For this reason, it is crucial to find a hernia repair method which resolves mesh complications and minimizes recurrences. There should be a new and innovative operation that can be performed without using mesh.
Why direct suture?
The resolution to the aforementioned mesh problem is the direct suture closure of the hernia hole. As you can see above, even the use of a tough mesh still still leads to recurrences despite there being no ‘tension’. Why? It is because of the repair method which covers either the inside or outside of the hernia hole with mesh, leaving the open hernia hole untouched. There is always a possibility of the organs protruding again because the hernia hole itself is not directly closed. As a result, they could not fully prevent more recurrences even though they used a tough mesh.
Leaving the hernia hole open also accounts for the high rate of recurrences for old-fashioned tissue repairs, which used to be around 10-30%. Tension is of course an issue, but the major reason for high recurrences is from lack of directly closing hernia holes. A hernia is a disease that allows the intestine to escape through a hole in the abdominal wall muscles. So, if you block the hole firmly, it can be completely cured. That is common sense.
It is curious however that past hernia tissue repair methods ignored this common sense approach. And the same is also true of recent mesh hernia repair methods. Finally, after returning to our common senses, it’s clear to see that you need to find the hernia hole and close it directly. Then you can catch both rabbits, the recurrence issue and mesh complications. Thankfully, such a surgery was developed in 2012 at our Gipum Hospital. ‘Kang repair’ is the name of that operation. This is a new concept of hernia surgery and is the only one to perform direct closure of the hernia hole.
Direct closure of the hernia hole is not that easy because of the complicated anatomy around hernia holes. So, elaborate surgery is needed. A hernia hole is a gap between tissues that were originally attached to each other. So, even if you suture them together, there will be no tension, as they have been restored to their natural state. Therefore, by directly suturing the hernia holes, we can achieve the goal of using non-mesh and leaving no tension. It’s similar to the two birds and one stone analogy.
Kang repair, catching two rabbits
Kang repair significantly reduces the relapse and sequelae after a hernia operation. So far, more than 6,000 Kang repairs have been performed, with a recurrence rate of less than 0.5%. Mild and intermittent chronic pain have been the subject of complaints in less than 1% of cases.
All over the world, the side effects of mesh hernia repair are widely known to the public. Nevertheless, hernia surgeons continue to perform mesh hernia surgery as ‘the gold standard’ for the inguinal hernia repair. There are a lot of patients who are really frustrated by this situation. Whilst trying to find out if there were any other repair options so as to avoid mesh complications and high rates of recurrences, they came across Kang repair and came to Gibbeum Hospital from all over the world. They have discovered that the only way to solve the dilemma of inguinal hernias in this day and age is to undergo Kang repair surgery.
